CPAP compliance rates have been estimated as low as 17%1. Oral Appliance Therapy (OAT) offers an effective treatment option for mild to moderate Obstructive Sleep Apnea (OSA) and CPAP non-compliant patients. OAT keeps the airway open during sleep with a custom mandibular advancement device that is small, silent and most importantly, consistently used.

COMPLIANT WITH TREATMENT1
AVERAGE REDUCTION IN AHI9
CONTINUE TREATMENT AFTER 1 YEAR10
CONTINUE TREATMENT AFTER 4 YEARS10
While CPAP has been shown to be more effective at reducing polysomnographic variables in lab settings, due to the higher compliance rate of OAT, it has been shown to be as effective2 treating real world health outcomes like:
A 2012 study found a substantial decrease in daytime sleepiness in patients using oral appliance therapy4.
A 2021 study found Quality of Life significantly improved in patients treated with oral appliance therapy. There was a mean difference of 1.8 points on the Functional Outcomes of Sleep Questionnaire (FOSQ), following treatment with an oral appliance5.
A 2012 study found that cognitive functions improved on all performance measures after only 6 months of treatment with Oral Appliance Therapy 4
A 2013 Meta-Analysis found that across 7 studies there was significant evidence that Oral Appliance Therapy had positive effects on pre- and post-treatment systolic, diastolic, and mean arterial blood pressure6.
A 2015 study found that oral appliance therapy improved on serum levels of nitric oxide derivatives and endothelial function by endothelium-dependent flow-mediated dilation (FMD) in obstructive sleep apnea syndrome (OSAS)7.
A 2013 study found oral appliance therapy may be equally effective as CPAP in reducing the risk of fatal cardiovascular events in patients with severe OSA8.
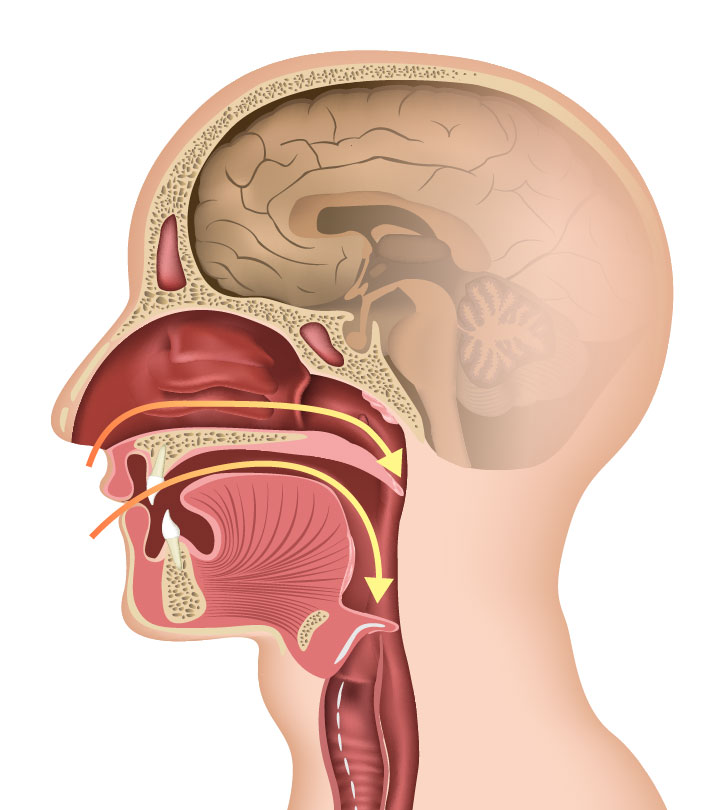
Oral appliances for Obstructive Sleep Apnea are custom made to fit your mouth. They work by gently repositioning the lower jaw to prevent collapse of the airway during sleep.

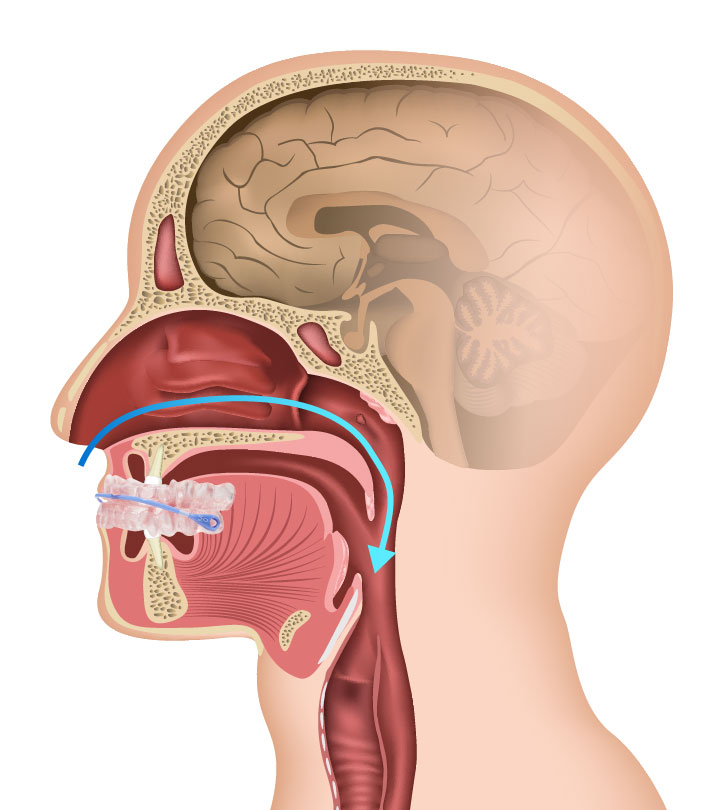
Each oral appliance is custom-made to fit. A TreatOSA4VA dentists begins by measuring the patient’s therapeutic bite to determine the optimal starting position of the appliance. 3D scans of your teeth are used to ensure the device fits securely and comfortably. The bite measurements and scans are sent to a dental lab which fabricates the appliance. Once complete it is sent to your TreatOSA4VA provider, who schedules an appointment to fit and adjust the device. Follow up sleep testing is scheduled to ensure the appliance is working effectively. It may be necessary to periodically adjust your appliance as your body adapts.


1.When adherence is defined as greater than 4 hours of nightly use, 46 to 83% of patients with obstructive sleep apnea have been reported to be nonadherent to treatment. Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc 2008; 5:173.
2.The objective mean use rate was 6.4 +- 1.7 h/night at 1 year follow-up in continuing users, with a regular use rate of 83%. Dieltjens M, Braem MJ, Vroegop AVMT, Wouters K, Verbraecken JA, De Backer WA, Van de Heyning PH, Vanderveken OM. Chest. 2013 Nov;144(5):1495-1502. doi: 10.1378/chest.13-0613.
3. Head-to-head trials confirm CPAP is superior in reducing OSA parameters on polysomnography; however, this greater efficacy does not necessarily translate into better health outcomes in clinical practice. Comparable effectiveness of OAm and CPAP has been attributed to higher reported nightly use of OAm, . Sutherland K, Vanderveken OM, Tsuda H, Marklund M, Gagnadoux F, Kushida CA, Cistulli PA, Oral Appliance Treatment for Obstructive Sleep Apnea: An Update. J Clin Sleep Med. 2014 Feb 15; 10(2): 215–227.
4. Tegelberg A, Wilhelmsson B, Erixon-Lindroth N, Lindström LH. Improved cognitive functions after treatment with an oral appliance in obstructive sleep apnea. Nat Sci Sleep. 2012 Aug 22;4:89-96. doi: 10.2147/NSS.S33849. PMID: 23620682; PMCID: PMC3630975.
5. Rangarajan H, Padmanabhan S, Ranganathan S, Kailasam V. Impact of oral appliance therapy on quality of life (QoL) in patients with obstructive sleep apnea – a systematic review and meta-analysis. Sleep Breath. 2022 Sep;26(3):983-996. doi: 10.1007/s11325-021-02483-0. Epub 2021 Sep 13. PMID: 34515959.
6. Iftikhar IH, Hays ER, Iverson MA, Magalang UJ, Maas AK. Effect of oral appliances on blood pressure in obstructive sleep apnea: a systematic review and meta-analysis. J Clin Sleep Med. 2013 Feb 1;9(2):165-74. doi: 10.5664/jcsm.2420. PMID: 23372472; PMCID: PMC3544387.
7. Lin, CC., Wang, HY., Chiu, CH. et al. Effect of oral appliance on endothelial function in sleep apnea. Clin Oral Invest 19, 437–444 (2015).
8. Anandam A, Patil M, Akinnusi M, Jaoude P, El-Solh AA. Cardiovascular mortality in obstructive sleep apnoea treated with continuous positive airway pressure or oral appliance: an observational study. Respirology. 2013 Nov;18(8):1184-90. doi: 10.1111/resp.12140. PMID: 23731062.
9. Marklund M, Verbraecken J, Randerath W. Non-CPAP therapies in obstructive sleep apnoea: mandibular advancement device therapy. Eur Respir J. 2012;39(5):1241–1247.
10. Sutherland K; Vanderveken OM; Tsuda H; Marklund M; Gagnadoux F; Kushida CA; Cistulli PA; on behalf of the ORANGE-Registry. Oral appliance treatment for obstructive sleep apnea: an update. J Clin Sleep Med 2014;10(2):215-227.